Addiction Can Ruin Individual and Family’s Lives and Lead to an Early Death
Out of the 48.5 million Americans who had a substance use disorder (SUD), 80,391 of them died of a drug overdose (CDC 2024).
More about the Reward Deficiency Syndrome and Addictive Behaviors, Impulsive Behaviors, Personality Disorders, and Compulsive Disorders
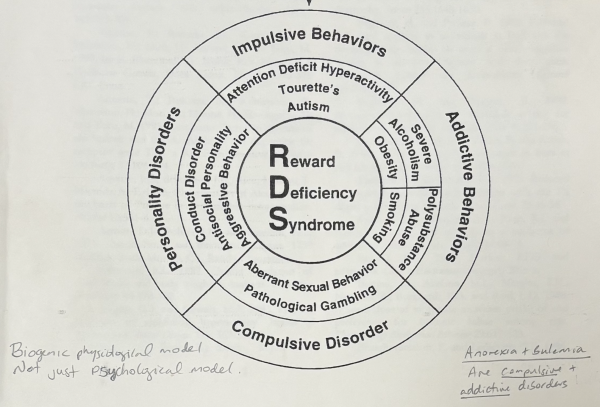
The “reward deficiency syndrome biogenic model,” which was originally described in 1997, appears in several journals, including the Journal of Psychoactive Drugs and Molecular Psychiatry around the year 2000. At the core of the concept is the brain reward cascade, which describes how chemicals in the brain must flow properly to reach a state of well-being. When that flow is blocked, reward deficiency syndrome develops. This condition is linked to a wide range of issues, including impulsive behaviors such as ADHD, Tourette’s, and autism; addictive behaviors such as alcoholism, obesity, smoking, or polysubstance abuse; compulsive disorders like OCD, pathological gambling, or aberrant sexual behavior; and personality-related disorders, such as conduct disorder, antisocial behavior, and aggression.
The research was originally studied by Dr. Kenneth Blum, and later expanded upon with Dr. J. Holder. Together, they explored how disruptions in the brain reward cascade contribute to reward deficiency syndrome. They later founded organizations, such as the American Academy of Addiction, and conducted influential research published in leading psychiatric journals. Dr. Holder also asked an important question: could tonal chiropractic care influence the brain reward cascade? Since some of the receptors involved in this cascade extend down into the spinal cord, the theory was that spinal subluxations could regulate the system. If that were the case, neurologically based chiropractic adjustments could restore proper flow and reduce reward deficiency syndrome.
The results of their research were breathtaking. They conducted studies on addiction patients, comparing standard residential treatment, standard treatment plus chiropractic care, and standard treatment plus placebo. The group that received true tonal chiropractic care- specifically torque release technique- showed a 100% retention rate over a 30-day residential model. This was so significant because of the 50% attrition rate in in most studies. Participants also experienced improvements in anxiety and depression, reduced nursing station visits, and overall better treatment outcomes compared to controls.
The mechanism involves the limbic system, dopamine pathways, and opioid receptors, all of which are part of the brain reward cascade. One-third of the limbic system extends into the spinal cord, which explains the direct connection between tonal chiropractic and its influence on the cascade. By correcting subluxations, practitioners can restore proper neurological flow, reduce reward deficiency syndrome, and improve outcomes for patients struggling with addiction and related disorders. In order to properly address these disorders, it is essential to accept that the common denominator is the spine, spinal cord, and mesolimbic brain centers. These areas of the nervous system must be free of tonal subluxation.
Dr. J Holder has applied this approach for decades at the Exodus Addiction Center in Miami, treating patients with a wide range of addictions and achieving results far superior to standard methods. Assessing for subluxations involves specialized testing beyond traditional orthopedic palpation, such as VNC testing, which evaluates nervous system function. Treatment then focuses on activating areas that are neurologically stressed or subluxated, firing new information into the spinal cord and brain, and restoring healthy function over time.
Ultimately, when the brain reward cascade is restored, patients experience a higher state of well-being, reduced compulsions and addictions, and improvements in conditions such as ADHD and OCD. This approach, rooted in the neurobiological medicine model, begins with addressing nervous system stress overload and correcting it to reduce reward deficiency syndrome
- Dr. Kenneth Blum, PhD (Pharmacology, New York Medical College; MS Medical Science, New Jersey College of Medicine; BS Pharmacy, Columbia University)- Neuroscientist who coined the term Reward Deficiency Syndrome (RDS) in 1995; professor of pharmacology at the University of Texas Health Science Center until 1995.
🔗Kenneth Blum – Wikipedia
🔗 MDPI Journal on RDS - Dr. E. R. Braverman, MD- Physician and researcher in neuropsychiatry and addiction medicine; co-author with Blum and Holder on the landmark paper Reward Deficiency Syndrome: A Biogenetic Model (2000).
🔗 PubMed – Journal of Psychoactive Drugs (2000) - Dr. Jay M. Holder, DC, CAP, DACACD (Doctor of Chiropractic; Certified Addiction Professional; Diplomate of the American College of Addictionology & Compulsive Disorders)- Developer of Torque Release Technique®; founder/director of the Exodus Addiction Treatment Center (Miami); adjunct professor and award-winning researcher in chiropractic and addictionology.
🔗Torque Release Research PDF
🔗Balance Atlanta – Addiction & Chiropractic
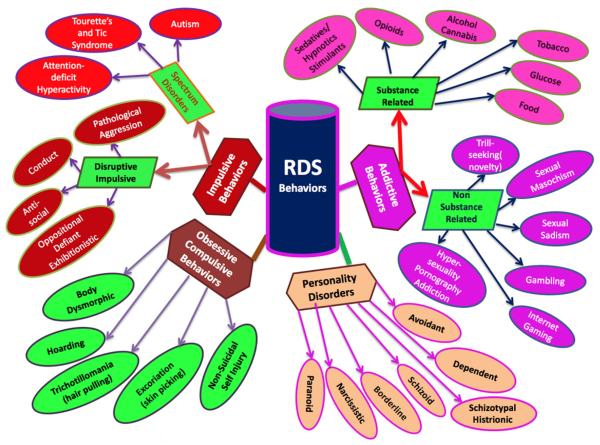
RDS can show up in many different ways, ranging from impulsive behaviors (like ADHD, aggression, or conduct issues) and obsessive-compulsive behaviors (such as hoarding, skin-picking, or self-injury), to addictive behaviors (including drugs, alcohol, food, gambling, or internet gaming) and even certain personality disorders.
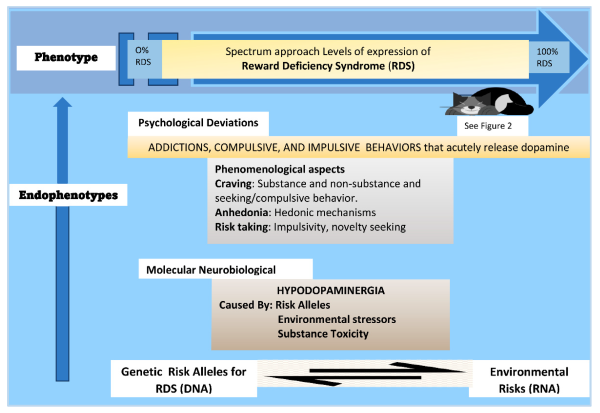
RDS develops along a spectrum—from mild to severe—based on a mix of genetic factors, environmental risks, and neurobiological changes. At the root is something called hypodopaminergia, meaning the brain doesn’t release or respond to dopamine efficiently. This can cause problems like craving, anhedonia (inability to feel pleasure), and risk-taking/novelty-seeking behaviors. To cope, individuals often turn to substances or compulsive actions that provide short-term dopamine “hits,” reinforcing the cycle.
Both figures from the article Reward Deficiency Syndrome (RDS) Surprisingly Is Evolutionary and Found Everywhere: Is It “Blowin’ in the Wind”? Journal of Personalized Medicine, 12(2), 321. https://doi.org/10.3390/jpm12020321)
Understanding the Science Behind Reward Deficiency Syndrome and Addictive and Compulsive disorders
- Craving and addictions are a malfunction of the reward centers of the brain involving the neurotransmitters and the enzymes that control them
- Genetic glitches and epigenetic factors are both root functional causes
- The goal is to facilitate an adequate supply and balance of neurotransmitters, enzymes, brain chemicals to reach a state of well being and reduce the malfunction that triggers addictive and compulsive disorders
- The nervous system must be viewed from a tonal functional model in order to fully understand the issue. The tonal nervous system (aka central integrated state) can be viewed like the rhythm of music. A good tone= Mozart (lower allostatic stress load) vs bad tone= out of sync and off beat (high allostatic load).
- The tone, or allostatic load, of the nervous system, can be measured, quantified and tracked over time. A vital baseline assessment is essential to manage a patient correctly. Specific bloodwork and genetic testing can also provide valuable insight to the tone of the nervous system.
- Stress overloads the nervous system and creates a high allostatic stress load. This is the same thing that creates tonal subluxations. Stressors can be physical, chemical, mental/emotional, or environmental.
By incorporating a comprehensive Neuro-Biomedicine model, which incorporates nervous system tonal care, cellular energetics, lifestyle modifications, food immune reactions, and essential nutraceuticals, we can provide the best opportunity for recovery, remission, happiness, and productive successful days, months, years, and life ahead. This individualized approach is the key to our beyond outpatient care program.
American College of Addictionology & Compulsive Disorders: Reward Deficiency Syndrome (2025)
Torque Release Technique Certification (2007)
American Institute of Stress (Fellow)
International Association of Functional Neurology and Rehabiliation